How much does an EHR system cost?
The cost of EHR software can range from $600 to $1200 per year per user. This electronic health record cost includes software licensing, setup cost, training cost, and maintenance cost per user.
Depending on the vendor, you can either get a subscription model or a perpetual license. Some of the top EHR to use are Epic, Athenahealth, Cerner, and eClinical.
But if you opt for a customized EHR, expect to pay from $50,000 to $150,000 of upfront cost. It is the total of infrastructure (hardware and development tools), human resources (developers, PM, tester) and deployment cost (training, integration). Some projects can cost more than $150K with a complex scope.
However, the EHR implementation cost can vary based on where you hire the developers. For examples, an US developer require $40 to $70 per hour, while a Vietnamese developer only take $20 to $50, with the same code quality.
You can guess that SaaS is definitely cheaper than a customized one. But surprisingly, based on many research, SaaS usually led to much higher TCO over the year while driving less ROI. Read on to learn our EHR cost breakdown and ROI analysis
EHR implementation cost breakdown
To help you estimate your budget more accurately, here are the factors affecting the final EHR implementation cost.
1. Number of features and users
- Number of features: Each EHR will have different features, from basic to advanced, serving small clinics to enterprise-level needs. Especially with customized EHRs, you can request specialized modules crafting to fit your process requirements and your facility’s needs. For example, if you need to integrate AI for better data analytics, prepare a higher budget for that addition.
- Number of end users: This determines the licensing fee, training cost, support cost, and IT hardware budget. You should also prepare capital to onboard new users in the future.
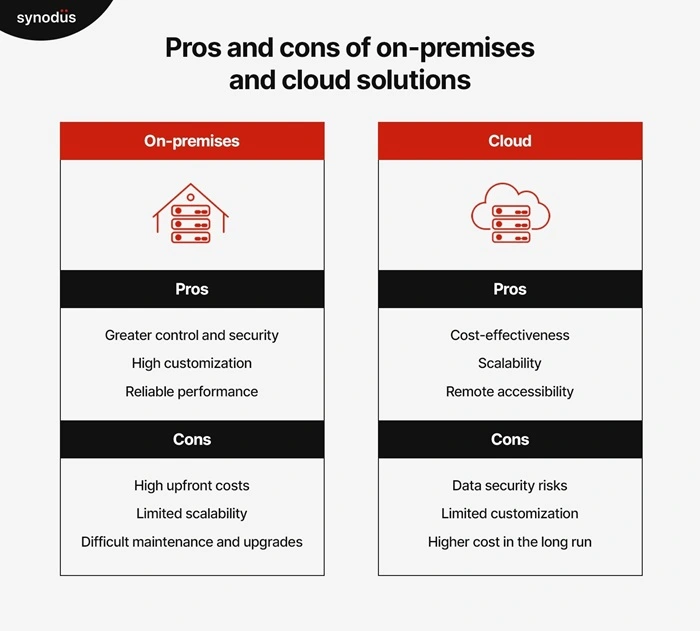
2. EHR deployment model: Cloud or on-premises
The EHR deployment model makes a big difference in production costs.
A cloud-based EHR will be hosted and run on the vendor’s system. The vendor will take care of all operations, bug fixes, and updates. For on-premises, you will pay additional costs for setting up and managing the server.
The average upfront cost for setting up a cloud-based EHR is $26,000, meanwhile it’s $33,000 for an on-premises. Yet, the latter offers high security, great scalability, and better adaptivity, leading to a much lower TCO over 5 years.
3. Implementation support
EHR implementation cost for support accounts for 15 to 20% of the total cost. This may be a surprising number, but with the help of experts, the implementation will be faster, and the system will be better exploited, so it will be beneficial in the long run.
According to the Medical Group Management Association, the average hourly cost of EHR implementation support in the US is:
- Project management: $100-$200 per hour
- System configuration: $150-$300 per hour
- Data migration: $50-$200 per patient record
- Training: $50-$150 per hour per trainee
- Go-live support: $200-$500 per hour
The price can be x2 and x3 times lower in regions such as Vietnam, India, Malaysia, or Mexico.
4. Interoperability costs
Your EHR should be able to:
- Seamlessly transfer data between departments, providing accurate and timely data for the right diagnosis.
- Can communicate and coordinate well with other facilities, especially for healthcare franchises with clinics across a region.
The more third-party tools you want to integrate, the higher the electronic health record cost. Especially the latter, as it’s more complex to deal with.
5. Training cost
Introducing a complex system to a hospital will cost training for doctors, pharmacists and hospital staff. Training costs will vary depending on the number of features, the system’s complexity, and the hospital’s size.
6. Maintenance cost
Maintenance costs, including the cost of repairing, upgrading, and adding modules to optimize performance and lower costs, must be considered before implementing an EHR.
Calculating the ROI of EHR for small and large facilities
Return on investment (ROI) is a way to estimate if your EHR adoption is a success or failure by calculating the ratio between net income and investment. You can use ROI to consider the cost benefit analysis of EHR implementation.
In healthcare, ROI can be expressed directly through increased recurring revenue for the organization or in less quantifiable terms, such as staff satisfaction, more efficient clinical processes, and reduced time spent on paperwork.
In a study with US doctors, healthcare staff, and physicians:
- 94% reported that medical records are always available and updated in real-time when needed.
- 88% reported that EHR offers clinical benefits.
- 75% reported that EHR allows them to deliver better patient care.
- 63% of patients reported no errors in medication.
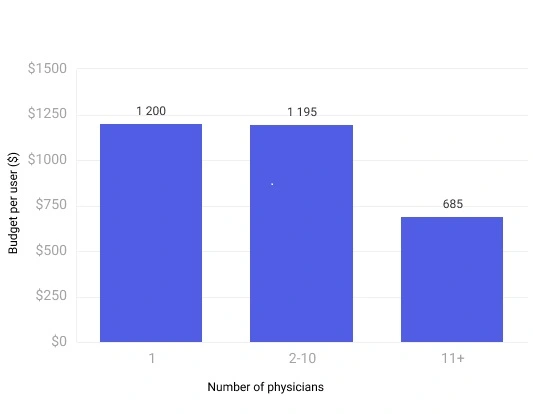
However, Software Path showed that the larger the healthcare practice, the less money they spend on EHR per user and a better return. Meanwhile, the average cost of EHR system is too expensive for small practices. The cost of managing it might exceed the actual value. In this case, an EMR is a much better choice.
Your choice of deployment model also leads to different ROIs based on HealthIT. A SaaS has fewer upfront costs, but its five-year TCO can be x5 or x10 times higher. Meanwhile, a custom-made system can yield a higher ROI faster despite requiring a large initial investment.
How long will it take to recover my EHR investment? For small and solo facilities, it would take at least 2.5 years to see a positive ROI. For primary care practices, it would take around 10 months. For large hospitals, the time can be shorter.
Optimizing the electronic health record cost
EHR implementation costs can be high, and its ROI might be unclear. But there are always ways to maximize your spending. Before making any decisions, consider these tips to bolster a cost-effective and high-quality EHR.
1. Using open-source EHR or open-source development tools
If you go down the SaaS route, open-source EHR such as OneTouch EMR, OpenMRS, or Solidmed can be a great start. These tools are cost-effective and constantly upgraded, but they might be limited in advanced features. We only recommend this strategy for small clinics.
However, using open-source development tools is an effective option for a customized EHR. These tools are highly flexible, with a price range from free to affordable. You can add open-source tools to your tech stack, combining them with closed-source ones to ensure high security and minimize their ugly side effects.
At Synodus, our tech stack contains both open-source, closed-source to low-code tools, all of which are cost-effective tools to build an EHR. By providing an extensive selection range, our clients can pick out what suits them best.
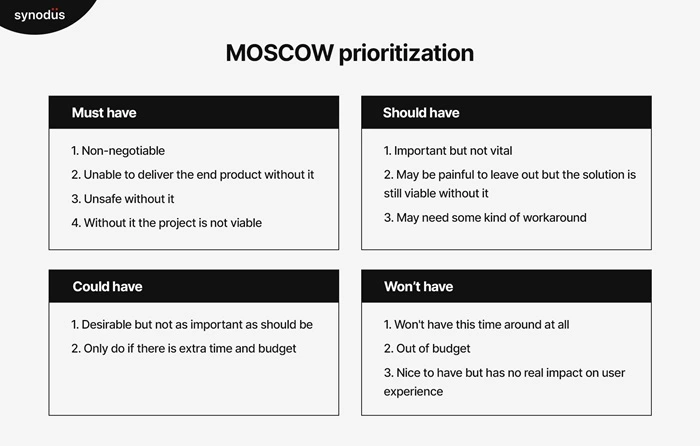
2. Create a list of prioritized features
Having an EHR with all the latest and most advanced features is a dream, but it’s impossible. By identifying what core features to focus on, you can trim the fat on unnecessary features, make your EHR work with a tight budget, and ensure the EHR meets your primary and most essential needs.
This is when our senior Business Analysts work the closest with our client. The key is to understand your facility’s challenges and wishes.
3. Compromise on security
Loss of data or information breaches will fine your facility some hefty cash to recover. One way to reduce electronic health record cost is to cautiously consider security protocols first-hand before any hacks or threats can occur.
Find a vendor that emphasizes this and complies with multiple cybersecurity standards, data privacy protection, and regional regulations. They should also be well-versed in using tools for firewall testing and security checking.
Understanding this, our team utilizes HIPAA, HL7, GPDR, and ISO to make sure your EHR complies with global standards. For local ones, we take time to deep dive and learn your culture, which we did when building EHR for Islamic countries such as Malaysia.
4. Use packaged solution or white-label EHR: cost-effective + customization
If a SaaS tool lacks flexibility and fully tailored software is too expensive, a packaged or white-label EHR can easily balance those two dimensions.
Both packaged and white-label solutions are pre-built solutions containing standard features for all healthcare facilities. However, they also leave room for customization, allowing you to create a tailored solution while reducing the time spent setting up the fundamentals.
Thanks to this, you can save money and resources instead of building from scratch, reducing the cost of electronic health records. This symmetry is favored by many healthcare facilities.
Not just a custom EHR development provider, we are also the top vendor of packaged and white-label EHR in APAC.
5. Looking for an experienced vendor
First and foremost, an experienced vendor does not necessarily mean a high-priced or famous vendor.
A vendor with top-notch technology and market knowledge will provide you with the most suitable solutions by offering cost and performance optimization options and advising on solutions during the implementation process. With experienced vendors, communication and system implementation will be faster and more efficient, cutting down on additional costs.
Looking through their portfolio and testimonials to find a similar case to yours is one way.
A vendor, like Synodus, who has served 30+ healthcare facilities and 10,000+ staff, for example, can be a good start!
You deserve a Cost-effective, Secure & High ROI EHR today
Wrapping up
It’s a sure thing that hospitals gain great benefits from using EHRs. Yet the electronic health record cost isn’t the breeze for many. To optimize your investment, the key is to understand the causes of their high price, learn how to optimize your spending, and find a suitable vendor.
How useful was this post?
Click on a star to rate it!
Average rating / 5. Vote count:
No votes so far! Be the first to rate this post.