Why implementing EHR is a hurdle for many facilities
You must have heard words like “seamless, smooth, or intuitive” in every marketing of EHR. While the software appears to be so, the process of implementing it does not. One wrong step can lead to a failed adoption, wasted money, lost time, and more time to recover from it.
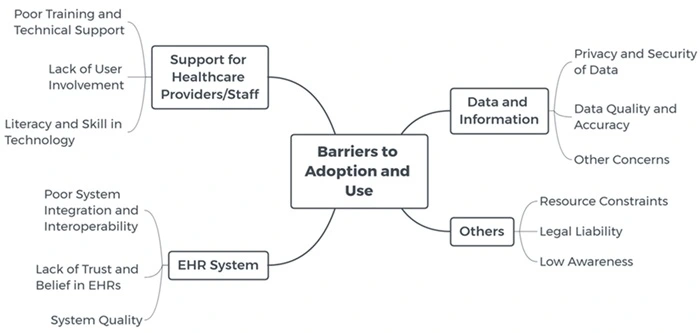
So, why are there so many EHR adoption challenges?
All staff must onboard with the idea
The end-users of your EHR are the doctors, nurses, and administrative staff. However, what they gain from the EHR implementation is different. The key is to ensure that despite all the contrasts, your staff must accept the EHR and understand what change it can bring to their daily work.
Step 1: There must be a clear and precise description of the EHR features that can handle their requirements. For example, doctors need an automatic test results update to aid their diagnosis. But the administration needs a digital platform to create the e-profile at reception, instead of printing paperwork.
Step 2: Conduct a training session to teach them to utilize the EHR correctly. At the same time, you should identify and resolve any initial issues. This will lay the groundwork for successful long-term implementation.
Modification in technical specifications
EHR implementation can be complicated by numerous tech hurdles. Before fully adopting EHR, your IT personnel must thoroughly test all EHR iterations to ensure they are complete. This stage involves checking the compatibility of hardware, software, and network interfaces when a telemedicine element exists. They must also prepare backup and downtime procedures and access credentials.
11 strategies to deal with EHR implementation challenges
Here are some steps that you can take to minimize the challenges, stay ahead of the current, and bulletproof your EHR adoption.
1. High cost
The most vibrant challenge in EHR implementation is its cost, which many practitioners are afraid of going over budget. The average price for an EHR can range between $20,000 to $70,000, with some reaching up to 100,000+ based on complexity.
While some providers may offer SaaS solutions with cheaper starting rates, the yearly price and TCO after 5 years are always the headache. It might be affordable at first, but with all the hidden costs, you end up paying more than for a customized one. We have explained it in this EHR cost breakdown.
One solution is to prioritize the basic set of EHR features first to solve your facility’s main problem. Afterward, you can upgrade it with more specialized features.
Another solution is to consider a tailored EHR from the start. Healthcare is a complex industry with many regulatory and cross-processes, and a commercial EHR might not be efficient enough to handle this niche.
For those with a tight budget, open-source EHRs with limited feature sets are an option. However, these systems can lead to unstable security compliance, which is when a more expensive certified solution becomes more economically viable.
2. Hidden cost of workflow disruptions
During the transition between the legacy system and the new EHR, your staff will spend time training and getting used to integrating it into their workflow. This, of course, takes away their time for the main task.
The challenge is that you can’t skip this step. It’s important that your staff adapt well to the new EHR system. So, how can you build an effective training that isn’t being expanded and costs more money on operational interruptions?
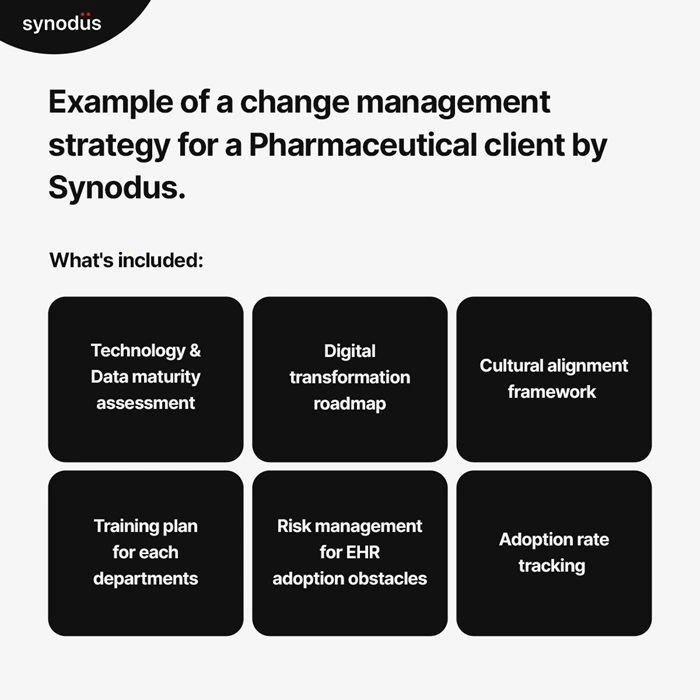
One way is to build a specific-to-detail change management strategy. Another attempt is initiating pilot tests in specific departments to see how the EHR fits. Your staff can help each other out later instead of relying on the vendor or IT departments entirely.
Minimizing downtime for training is also suggested to reduce disruptions to patient care. This can be achieved through developing extensive online training sessions, tutorials, and ongoing support.
3. Issues with IT infrastructure
Most healthcare leaders worry if their IT infrastructure is strong enough or whether they have enough hardware to work with an EHR. Meanwhile, the IT team is worried about the skills it needs to deal with connectivity issues, data migrations, and security. If not dealt with immediately, they can cause multiple delays and require additional resources to resolve.
This can easily be prevented early on by carefully assessing your infrastructure’s support capability, performance, and availability requirements for EHR system integration.
Another way is to outsource an experienced IT consultant. They can perform a thorough assessment of the existing infrastructure and identify gaps or deficiencies before the implementation. They also assist with system integrations, data migration, and connectivity issues to make sure the EHR implementation goes smoothly.
4. Data migration
As the most time-consuming and tedious process of EHR implementation, this challenge is undoubtedly a big eye roll for many facilities. Not to mention, while migrating data from one place to another, private and sensitive information is exposed to the risk of being leaked or lost. This is another EHR implementation challenge to be mindful of.
Those same data must be migrated accurately to prevent disruption of patient care. The best way is to start with the most recent files and gradually move on to the files at the back.
You should also assign someone to upload all the new faxed and paper-based information. That information must be stored properly to facilitate everyone’s use of the new EHR system.
5. Data governance, security and privacy protection
Next on the list are the three musketeers many facilities are concerned about: governance, security, and privacy.
Unlike the above, these data-related EHR implementation challenges happen after the deployment, not during it. They are data breaches and a firewall that is too weak to keep all the files safe, especially for a growing database. With so much sensitive information, including personal information, health data, and insurance claims, healthcare has many security and data standards.
It is also crucial that the data remains relevant and accessible. Healthcare facilities should seek clarity on the privacy measures and protocols that will be integrated.
In addition to the software’s inherent qualities, a robust data governance strategy is essential. This strategy will guide healthcare organizations in properly handling patient data, including its acquisition, storage, transfer, and disposal. Furthermore, all personnel within each healthcare organization and facility should thoroughly understand their organization’s strategy and know how to adhere to it effectively.
6. Challenges with EHR interoperability
50% of senior healthcare finance executives agree that interoperability is their biggest worry.
It happens to doctors struggling to transfer data during pandemic manually and continues until now. The whole process is prone to errors, duplicates, and clinical dissatisfaction. This can result in untimely or inappropriate clinical decisions, causing delays in diagnosing and treating patients since they do not receive timely patient history.
Another EHR implementation challenge is doctors’ doubts about EHR software’s ability to streamline provider or department interactions.
Given all the issues, hospitals and health organizations should consider interoperability at the beginning of EHR implementation and weigh all the interoperability options they intend to adopt. Hiring a consultant and integration services provider is advisable to ensure the safe incorporation of the EHR system into the healthcare IT ecosystem.
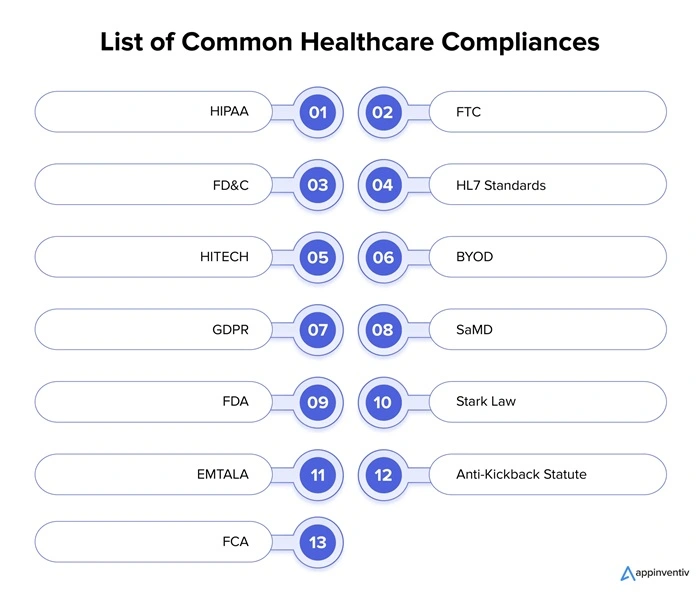
7. EHR not comply to regulatory standard
Challenges with EHR interoperability also arise regarding regulatory compliance and reporting. EHR software providers must ensure the compliance of their products with various healthcare regulations and reporting requirements (HIPAA, Meaningful Use, PQRS). Healthcare organizations require a straightforward compliance procedure, and the EHR system must be well-modified to meet those requirements.
The first step you can adopt is to build a compliance team that administers EHR-related regulations and reporting. The team shall implement standardized data collection and reporting practices. At the same time, health facilities keep up with changes in healthcare regulation and adapt EHR systems accordingly.
8. Staff resistance
Implementing new technology, like EHR, is often opposed by people within the work environment. This resistance can go from clinical-level staff to the board members and stakeholders. Therefore, a good “marketing” strategy is needed to help EHR implementation win over.
To deal with this obstacle in EHRs implementation:
First, you must build acceptance and positivity around the changes for healthcare staff. This can be done through a slow yet steady implementation and a comprehensive training plan.
Make sure that the EHR system maintains the same working hours or even saves time for practice staff. After all, staff need to understand that adopting EHR means a better business model and improved job satisfaction.
9. Unsuitable user interface design
Another significant EHR implementation challenge is the user interface (UI) design mismatch. It’s not that your doctors and healthcare staff are “too old” or “stubborn” to learn about technology. The truth is they are too busy to figure out how to use an app. If it’s too complex to navigate, they will be frustrated.
Choose an EHR with user-friendly and navigable interfaces. You can gather a group of end-users to participate in the design process, testing the usability and quality of the EHR system. They will examine whether the EHR system has efficient data entry and easy-to-use, disruption-free documentation features.
10. Lack of support and communication from vendors
The support and communication from vendors play a pivotal role in the success of EHR implementation. Without proper communication, the goals cannot be met, thus creating more EHR challenges in integrating the data collection system and training the staff.
It’s recommended that effective communication be maintained between the healthcare provider, IT vendor, and patient during the building of the EHR system. Connection and communication between parties must remain continuous to satisfy all parties’ expectations.
Also, healthcare facilities should appropriately address the provider’s concerns and feedback, and the vendor should be able to build effective tools as required by the provider.
11. Lack of planning and management
Setting up a clear plan and proper development roadmap from design to post-implementation will help you avoid many EHR challenges. Yet, many skip this step, thinking they can figure it out later during development.
Solving this electronic health record implementation challenge, you should strategically plan it first, with all stakeholders and staff committed seriously to it. This can prevent any future cybersecurity threats and possible incidents.
What should be included in a good plan?
- Straightforward requirements and a list of features.
- A software architecture showing how those features are built and connected.
- A development roadmap that breaks down each milestone, with who’s in charge, how many people are taking part in the sprint, the deadline, and the promised delivery.
So, should I invest in an EHR?
Just because some EHR implementation challenges exist doesn’t mean you should stop considering it. EHR will eventually be a great sidekick for every facility in this tech-demanding world. A good EHR can save up to $81 billion in annual cost for a large hospital facility.
Here are some of its great benefits that you should consider:
- For administration: EHR implementation digitizes and automates the error-prone and time-consuming administrative tasks. For example, when a patient’s appointment is scheduled, the schedule is linked to the progress note, and the system automates billing, coding, prescription refills, manages claims, etc.
- For doctors: They can give more accurate and timely advice or diagnosis thanks to updated digital records.
- For facility operation: Better communication among departments and facilities (for franchise healthcare brands) by transmitting medical data records. For instance, cross-facility doctors can check patient’s health records for current medication and allergies to alert other medical teams of potential conflicts during treatments.
- For patients: Patient portals allow them to access all their medical records, lab tests, and results. This enables patients to become more active in their care solutions, gaining more positive results in overall health and increased satisfaction.
One of the best solutions you can opt for right today is Work with an EHR expert for consultation.
At Synodus, we have worked with 30+ healthcare facilities in customizing a EHR to their unique needs and regulatory. With extensive research on your business requirements, we will advise on your EHR architecture, features, and build a plan to avoid all the EHR implementation challenges mentioned.
And the best part? We can figure out an EHR that checks your scope, checks your quality, and checks your budget.
Wrapping up
So far, it is inevitable to face certain EHR implementation challenges. It could be hidden costs, concern about security and interoperability, or staff’s reluctance to adopt the new system into their workflow. However, those issues can be resolved with a clear, steady integration process with security standard compliance, privacy protection, and better planning and management.
How useful was this post?
Click on a star to rate it!
Average rating / 5. Vote count:
No votes so far! Be the first to rate this post.




